
The CMTA hosted a very informative talk on Zoom in September, 2020 to the CMT community featuring well-known orthopedic surgeon, Dr. Glenn Pfeffer. I’ve transcribed this talk for you! Enjoy!
Elizabeth Ouellette: Welcome Dr. Glenn Pfeffer. Dr. Pfeffer is the Director of the Foot and Ankle Surgical Program at Cedars-Sinai in Los Angeles.
I can’t tell you how much I appreciate and admire Dr. Pfeffer. He spends all his time with people with CMT. He wants to better their lives. He wants to see people walk. He has devoted so much time and energy to the CMT community. I am just so honored to have him here as a doctor, my son’s surgeon, as a friend and as a colleague. So welcome, Dr. Pfeffer, and thank you for coming on.
Dr. Pfeffer: Well, thanks for having me, and I’m surprised so many people came on a Saturday!
Elizabeth: First, I’d like to get to know Dr. Pfeffer a little bit more. And when I was doing some research on him, I saw that he did magic. I’m like, what surgeon does magic?
Dr. Pfeffer: Actually, magic is important to me. I did this through high school, college and medical school. I actually performed in nightclubs. I spent the summer in Nantucket at the Rose and Crown as their magician. And whatever it is that attracted me and still attracts me to magic, is the exact same feeling I get two weeks after surgery when a CMT patient is sitting in the office. Your foot’s going to be a little bloody. You’re going to have some sutures to take out, and we open up the cast, and you’ll see some pictures of this, and I hold their foot and I say, “Take a look here, your foot.” And it’s a new foot. It’s a foot they haven’t seen, perhaps ever, and the look on their face is identical to the look on people’s faces when you do a magic trick for them.
So whatever that is that attracts me is why I continue with magic. Magic is very simple you know. You can do things like this where you can take something and have it disappear. You can make it a little more complicated, which I do in the office for kids. You just take the same little piece of foam or whatever, and you just put it into this hand and you can just show people that it’s empty. So that’s sleight of hand, which of course is great for the magician. I still do this at orthopedic parties. But not to belabor it, if I were going to do this I wanted this to have the same absolutely startling response that people have with CMT when they see their new foot.
Elizabeth: Your father was a surgeon?
Dr. Pfeffer: He was a general surgeon.
Elizabeth: Oh and so is that what inspired you to be a surgeon?
Dr. Pfeffer: Yes, absolutely – I don’t think I’d ever have even gone into medicine if not from my dad’s influence. You know like all of us, I’m a mix of my dad’s DNA and my mom’s and they were very different people. But dad really inspired me with his surgery, and he was hard-working and I think it was my destiny. I probably have very little free choice in life. He didn’t make me but in terms of who I was, it was sort of my destiny, like the Jedi.
Elizabeth: You horseback ride or you did in the past. You scuba dive, you dance, you create bonsai, and I read somewhere you made a correlation between bonsai trees and surgery. Could you tell us a little bit more about that?
Dr. Pfeffer: I’ve always been interested in bonsai which are, you know, plants; they’re trees, and you keep them miniature by trimming their leaves, by trimming their roots, and you keep them in small pots. Everyone knows what they are, and what you do to shape them is you wire the branches and you hold them down so they look like a tree. And I realized only a year ago that what I’m doing with bonsai is identical to what I’m doing with CMT feet. I was sitting there in surgery and we were wiring a foot down and putting screw into it, and somebody who knew about bonsai said, “You know, Glenn, that’s exactly what you’re doing with bonsai.” And it was startling to me. You would think it would be obvious but it wasn’t.
As you may know I’ve got my own foot problem.
Elizabeth: I was just about to ask you; when you told me you had foot issues, I’m like, “He gets it.He knows what it is like to have a foot problem, and I think that’s a bonus for your patients.”
Dr. Pfeffer: Well I was just going to say, though, that’s how I got into horseback riding. Because I’m athletic by nature, but I couldn’t run. You know, I didn’t know what I had. It’s very poignant for me, the CMT world, because patient after patient, everyone who’s listening knows this, everyone, unless you had a mother or father who had CMT, you grew up not quite knowing what was wrong with you, right? And I didn’t either. I didn’t know I had a problem with my foot for 40 years. It sounds dumb, right? But if someone’s out there with CMT and no one told them they had CMT for 40 years, and they just thought they walked funny and they couldn’t keep up, and they were a little unbalanced, nobody would know. So I took up horseback riding because I could do what I wanted to do. I could fly through the air and jump, and I’m sure all the people listening have modified their lives in way so that they can function with their CMT.
Elizabeth: I think you can really relate to people with CMT and understand foot issues and the inability to do certain things.
Dr. Pfeffer: Well there’s no question, you know I don’t like to talk about it too much because you don’t want to get a little corny on a Zoom chat with all these people, but yes, I 100 percent relate to what people are going through. I’m not in a wheelchair. I don’t have problems breathing. My hands are strong. But for the isolation that somebody feels, the difference that somebody feels growing up with CMT, that is exactly what I felt for sure, and I don’t know that you can teach somebody that. I’m not sure you can really learn it, but it’s just in my soul. I’m not as bad off as most of the people with CMT at all but that’s why I get it, you know, that’s why I think it’s probably why I was attracted to all this.
Elizabeth: So why don’t we start your presentation, I think you are a fascinating person, and I know you’re an expert surgeon and the best of the best. And you’re also a great presenter, so I’m sure people want to hear what you do every single day.
Dr. Pfeffer: I want to just show you my world of CMT, and I have a certain kind of person that comes to me, right? Somebody who was unfortunately paralyzed in a wheelchair would not be getting to my office, so I do understand that I’m seeing a segment of the CMT population. But this is my world and what I go through every single day. At this point I’m confident that we at Cedars are operating on more CMT patients than anywhere else in the United States and we have a plethora of experience with it.
We’re lucky enough to have a large CMT program at Cedars with some of the most famous CMT neurologists on the face of the planet, such as Rich Lewis and Bob Baloh, and with amazing geneticists. If you have an issue, you can come to see the program. You’ll see a lot of people. Instagram is as alien to me as, you know, speaking Russian or French and yet it’s been a tremendous success for me and the people who follow it. I mean, my gosh, I didn’t even understand that at one point I had two people following it. Now we have close to 1400 people across the world, and I communicate with them all. It’s sad when someone from Ethiopia says “How can I come and have surgery?”, and of course the chance of them having surgery is almost zero for financial and travel reasons.
I encourage you to follow me on Instagram: #CharcotMarieToothSurgery

The foot’s complicated, right? It’s got a lot of muscles in it. There are 20 muscles in the foot, more than there is in the entire leg.
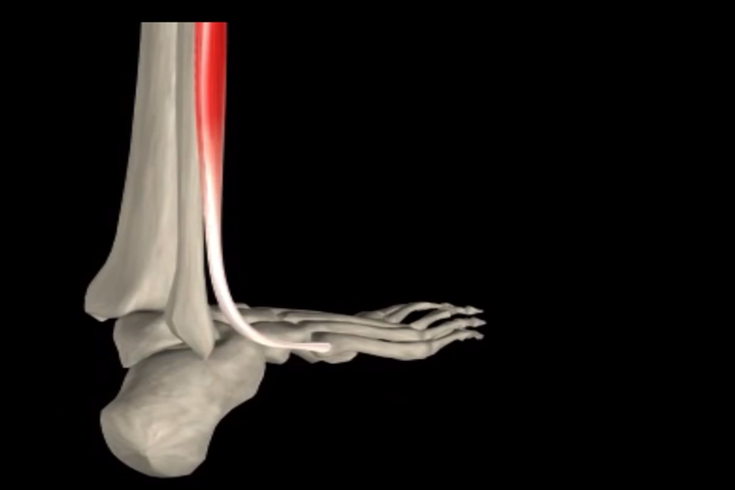
The tibialis anterior muscle is the strongest dorsiflexor (muscle lifting foot up toward the shin) and helps to lift the foot from the ground. The Tibialis Anterior Muscle also facilitates flexion of the foot upwards and extension of the toes. The Tibialis Anterior Muscle originates from the outer surface of the tibia and inserts into the first metatarsal bone in the foot which is located behind the big toe.
Above are the toe extensors. These are what lift up your toes, and interestingly with CMT, if the tibialis anterior that lifts your ankle gets weak, these toe extensors will start working harder, which is why so many of you will have a toe deformity. As the Tibialis Anterior muscle gradually weakens and the foot drops down, a contracture of the Achilles will occur because the tendon is no longer being stretched out during gait. The worse the contracture, the harder it is for the weakened Tibialis Anterior to lift (dorsiflex) the ankle.


Above is an image of the Peroneus Brevis, one of the key muscles that weakens in CMT. Why it happens exactly is still unknown, but this muscle, when it weakens, destabilizes the ankle and the foot starts to turn in, because this muscle is weak. And the other reason the foot starts to turn in so commonly is because this muscle in the right foot, looking from behind, stays strong.
So one weak muscle, and one strong muscle causes the foot to start to deform.
So let’s talk about that what causes the CMT deformity. I’m talking about this common cavovarus (very high-arch) foot. This is what happens every millisecond in our body. Muscles are pulling back and forth but keeping us balanced, right? With CMT, because of the paralysis that’s uneven, involving some muscles but no other muscles, they become weak. There is CMT. Some muscles are powerfully strong, and others are weak and that causes a deformity. It’s called a cavovarus, and you can really see it on this right foot.

If you took your hand, put it in your pocket and left it there for a year. Not only will you not be able to move it, you’ll probably never be able to open it up again because all of the soft tissue contracts. And that’s what you don’t want to have happen. If there’s one message I can give you, don’t let that happen.
The minority of patients I think benefit from surgery with CMT: Most patients do not need surgery.
The person below is wearing ground reaction force braces. This type of brace, made from carbon fiber or plastic actually bends and stores energy.
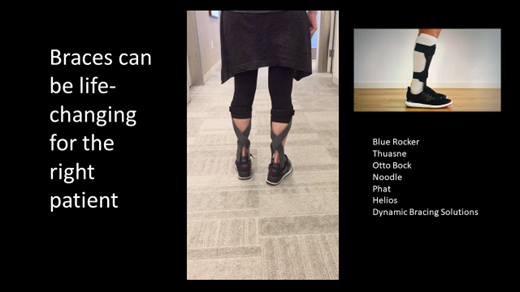
So when you have no function in the leg and the Achilles tendon isn’t working, these braces are just terrific. This person could walk a hundred miles if they had to because their foot’s flat on the ground and they’re doing great. Now, here are all the types of braces there are. Some are off the shelf. Some are custom made. Which is better than the other? I don’t know.
I absolutely think chocolate ice cream is the best. Does anyone disagree? Some people like strawberry or maybe vanilla, and the problem with the braces is you can’t try them all on unless you go to a spectacular brace shop, which I’m lucky enough to work with at our Center of
Excellence. Would anybody say that a size six dress of a certain brand is perfect for you? Of course not. You’d want to at least get it in the mail, try it on and send it back. That’s what you have to be able to do with braces. Unfortunately, we can’t try all these braces and some of them cost thousands of dollars, so try to go to a brace shop that has a wide selection to let you try some of them off the shelf.
Now that is not the right brace for a for this crooked foot. Some of you have it. I see this situation every day of the week. Would anyone put a foot like this into a brace? It’s like putting a square peg into a round hole. This is from Friday.

I was a little delayed today getting my talk all set because this gal just came in. She lives on a ranch. That’s the shape of her foot. That’s the shape of her brace. Shame on everyone taking care of her. Shame on her brace maker. She has pain walking on the side of her foot in a brace that looks like it’s something to a caged up an animal. That foot should never be allowed to walk the face of the Earth. That can be made flat, and even if this woman can’t get out of her brace, she can get into a brace with her foot balanced and her body weight plumb lined with no pressure walking on the side of the foot.
I can’t see you all, but how many of you have had or have a callus on the side of your foot? Right. That’s what happens. So these people should all have surgery, that’s how I feel. Now some people don’t want to wear a brace.
This is Katie’s Story
“Hi, my name is Katie. I live in Florida and I have CMT. Katie didn’t want to wear a brace. It was in sixth grade when I first started getting made fun of for the way that I walked and noticed that running and keeping up with my friends was becoming more difficult for me, and my parents started taking me to some doctors to try to find out what I could do to help me with my CMT. With each doctor that I met with, I felt like they didn’t understand my specific case of CMT. And they gave me some options, like braces and orthotics, and some of them would help me temporarily but nothing ever really helped me. So when I was in high school, I started falling almost regularly, and I missed out on my homecoming and my prom and just gave up on trying to find shoes that fit and started to become really discouraged.”
So Katie was a young woman, and she didn’t want to wear braces. She could have actually been in a brace. So she came from Florida. She said, “I don’t want to wear braces the rest of my life.” So I said okay and she had some muscles that were working. We operated on one foot, and she was incredibly brave and so we operated on the other. Katie could hardly walk without a brace without holding onto a wall.
Many of you know that kind of person. So the CMT type foot deformity is a tricky surgery. That’s the problem, right? People have had a lot of issues with it. There’s so many components to CMT surgery. The surgeries will take at least three to four and a half hours. There’s no way to get through it quickly. Basically, the failure of CMT surgery is when we don’t do enough.
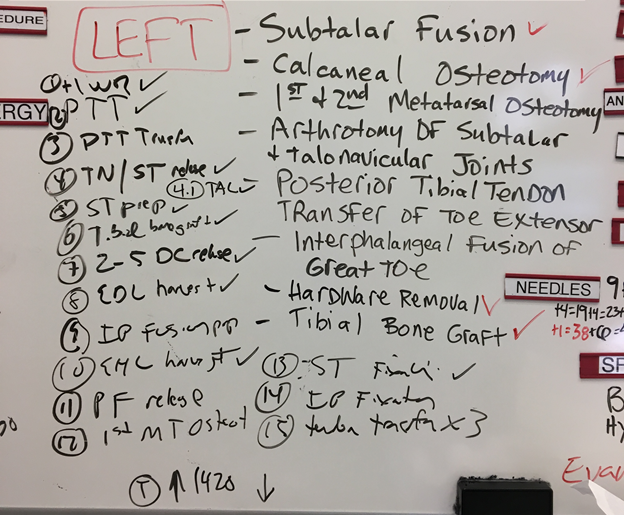
So this is what we put on the operative board at Cedars-Sinai. We put all the procedures someone’s going to have. “Hi, we’re going to fuse a part of your toe joint,” you’d say to a patient, “Okay, let’s schedule you for surgery. Hi, we’re going to do a tendon transfer on you. Okay let’s schedule you for surgery.” But the tendon transfers are some of the most complicated and extensive surgeries that there is in all of orthopedics except for some spine surgery or hip surgeries with dislocations and acetabular malformations.
Now how do we know what to do? Well, the problem is there is no good consensus on what to do. At least there hasn’t been, but we’ve done a lot of studies on this at Cedars and much thanks to the CMTA for their help.
This was a study we did. It was published in 2018. It was sponsored by the Charcot- Marie-Tooth Association (CMTA) and this was really incredible for us because we won a prize for this operation telling us how to correct the heel varus. And we won a prize for this as one of three research studies of the year most likely to change orthopedics. I just happened to have it here.
We took a print of one of my patient’s foot – Sarah. And we printed out 18 “Sarah’s”, 18 of these and then we studied them with different operations in the lab, but very exactly, and we showed which was actually the best operations for correcting heel deformities in CMT patients with her type of problem. Since then we’ve done other research more on heal osteotomies. We’ve looked at extensor transfers The most difficult, competitive organization in the world and the most academic is the orthopedic research society. And Max, who’s going to be joining us, he’s the second author, won a prize here just this past spring for a young investigator’s prize. I mean this is like winning a Nobel Prize in orthopedics and I was actually stunned by it. But part of the reason is because the whole area of CMT surgery is so poorly investigated, it’s not that hard to do some landmark work if you do the research.
Now there’s a big hole on how you should do CMT surgery and how it ends up in people and how do people do it. We’re just starting now. Some of you I’ve operated on. I always say I’m a pretty accessible guy and I don’t hear about too many people doing poorly. I know the ones I’ve had to re-operate on. I just spoke to a woman this morning where a young girl in New York is not having the motor strength that she needs. So I think I have a sense of it, but we’re going to study it and hopefully publish that by the end of the year.
So this was a remarkable thing – years in the planning. There were seven past presidents of the American Orthopedic Foot National Society and some of the most famous foot and ankle surgeons on the face of the planet, and with the sponsor of the CMTA sponsorship and Elizabeth’s fire in her belly. we brought these people together. And it almost killed me, literally, but we finally published a paper on our results, which just came out, and this is a consensus. We didn’t get everyone to agree, but I think just to sum it up here, this is accessible. You can get it through the CMTA and other places and if you’re going to have surgery locally in your area if you can’t come to Los Angeles for some reason, give this to your surgeon and say, listen I’m sure you know all about this but would you mind taking a look at this paper. And if they haven’t seen it they’ll be grateful to have it. https://www.cmtausa.org/news/breakthrough-guide-to-orthopedic-surgery-for-cmt/

Consensus Paper – Can be found on CMTA website: https://www.cmtausa.org/news/breakthrough-guide-to-orthopedic-surgery-for-cmt/
The goal of surgery is to give you a flat foot, and to balance your foot. My goal is to keep you out of a brace if I can, and I usually can if I’m willing to operate on you. It doesn’t always work that way, and if we can’t get you out of a brace, at least we’ll get you into a smaller brace. Much better to wear just a small piece of plastic than some of these bigger, bulky braces. So what do we do? We transfer tendons, which is moving muscle. We move strong muscles that are deforming the foot to weaker muscles which are letting the foot become deformed. We cut through the bone. Here you can see a bone. This is a right heel we’re looking at.
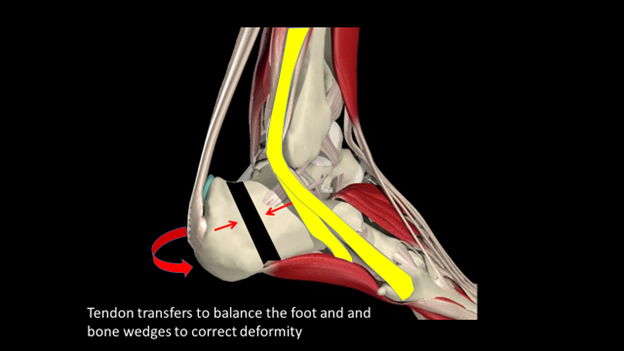
We take a wedge out of the bone. We twist the heel around. Here you can see it. So this is the heel from behind on the right side. You can see what we do. We take a wedge out and then we just simply shift the heel.

Okay, now who can you trust to do surgery? I hear there’s a lot of talk about me in chat rooms and stuff. I said, is there anything I ask my patients they don’t like. One person said, well you kept them waiting a lot, and another person apparently said, well, I just didn’t like him, but I guess he’s a good surgeon. But look out there. I don’t hear anybody saying about me, anyway, oh he sold me a bill of goods. He said I’d be good but I’m not. I just do not hear it. And if you do, tell Elizabeth and she’ll tell me because I want to hear about the failures I’ve had. I know the failures. I know why they’ve occurred but most of them have just been in the hands of God. Find someone who does at least one CMT surgery a month.

That’s a fair number of CMT surgeries to do. Most very experienced, busy surgeons will be doing three CMT surgeries, maybe two a year. But if you can find people around the country. that’s a good thing.
When should you do your surgery? Do it as soon as you know that you or your child can’t live with their foot the rest of your life. The sooner the better. Dr. K, my partner, because I don’t operate on people really under the age of nine, he just operated on a four-year-old yesterday from Utah, both feet. All these people are the perfect age for me to be doing surgery. You know, 10, 11, 15, 16, but you can do it anytime. It just gets harder because things get stiffer the older you are. So every day, because of Instagram, I chat with people. Some people are from Eastern Europe. Some people are from United States, and I have met most of them. I guarantee you I will make you better. I don’t know how much better. I’m not 100% sure I’ll keep you out of a brace, but I tell people you’re about a C-. I’ll at least get him to a B +. All right. So all I need is one strong muscle.
All I need is that muscle to move. That’s it. I just need any muscle. Is there risk? Of course.


The biggest reason surgery fails are that not enough was done. To do 18 surgeries at one time is a lot. T

Sarah was one of the most amazing. You may have seen her. She was 16. She couldn’t walk. We operated on one foot. All she said she wanted to do was walk down the high school aisle without having to hold on to her father. I called her years later. I said, “How are you doing? What’s going on with you?” And she said, Dr. Pfeffer, you don’t understand.” She said, “I just walked 10 kilometers around London with my boyfriend in cute shoes.” So that’s a magic trick all right. This gal, she said, “I don’t want to wear braces. I’ve had surgery. I’m going to be the first woman President of the United States. I’m going off to college.”
There she is. I mean, I can’t do that. Could she? She texted me a while ago. She goes, “After five or six hours of walking around campus, I need a little co-op brace. You know, ones that go into your laces because I get tired at the end of the day and sometimes need a little bit of help.” That’s better than I ever thought.

Q & A
I’m wondering how you deal with toes. Yeah it’s a great question. Very succinctly, toes are among the most difficult, actually, of surgery to do and the the longer people wait, the worse off they are. I can still fix the rest of the foot, but the toes become more and more problematic and there’s no easy answer for that. Sometimes as simple as just transferring the tendons. Sometimes we just cut the flexor tendons but I don’t like to do that in someone who has a motor disease. And what I’ve been doing lately with severe problems is we actually have been fusing these joints. It’s okay because the joints are useless. It’s not doing anything for anyone except getting in the way. So we fuse the joints and leave the tendons alone and and we can have some beautiful results with that. The problem is it’s a lot of surgery. That, in and of itself, that operation could take an hour, hour and a half. To add that onto a four hour operation … someone like the boy I’m operating on on Monday who has all that may have to come back, he may for the toe operation.
I had foot surgery, now my knee and hips are not aligned with my feet and I am having gait problems as well as some knee and hip issues. I’m wondering if that is because she waited too long and the CMT foot made her walk differently or do you do gait analysis beforehand? Have you heard of these problems? Someone has foot surgery. They get deconditioned and the hip muscles which are vulnerable to begin with, and the knee muscles get weaker, right? So they just get deconditioned. I know of one person in my career from Santa Barbara, and she had foot surgery. She was, you know, recovering and then she had that problem. You know, and all of a sudden her hips started to have a problem. It’s really really rare if the foot’s have been bad … feet have been balanced properly. My first thought is that the surgery didn’t work on the feet and that they’re imbalanced. The key is to remain conditioned, even if confined to a bed. Get some five pound weights on your ankle and lift up the leg.
Do you ever do both feet at the same time?
Never. You could do double surgery, like in a four-year-old like yesterday where Dr. K did that. Where you can just carry them around easily, but no, an adult is going to be completely impaired because they can’t put any weight on their foot for six weeks. Yeah. They would have to be tiny. Carry them around to the toilet. Carry them to the chair. What weight would that be? I don’t even know. You know, 50 pounds if dad’s strong.
Is there a particular age you recommend surgery?
There’s not a specific age, but how do you know to bring your child to trust you with his feet or her feet? When do you do it? Well, it’s absolutely the most important question anybody can ask, and I don’t have an answer. To operate on the crooked foot at any age, operate certainly on the young adolescent at 12 or 13, as soon as you know that person’s not going to live with that foot ideally for the rest of their life. If you look at your child, your friend, and you say I don’t want them to have that foot the rest of their life, that’s the time to have surgery.
Since CMT is a progressive disease do you do surgery and then 20 years later you have to do it again because the foot deforms or what is your experience with that?
There’s no literature on that whatsoever. The study that we started in 2017 will be coming to fruition soon. I said I told you, anyone I’ve operated out there please answer us when we write to you, and we’ll follow these patients along forever, and the only way anyone will have an answer for that is in 2037 when those patients are still around. Most … many of them … many of them were young and we’re going to find out how they’re doing but I can tell you this. If anyone’s considering surgery and they’re not doing well, don’t delay because someone says, tells you, you’re just going to be paralyzed in 10 years anyway. That’s not my experience. I’ve been operating for 30 years in California and no one has ever come back to me and said the operation hasn’t worked because I’ve gotten weaker, ever. And I’m around, you know, so I’ve never had that. So I don’t think these things progress. and I personally think that when you do this on a young person … this is really critical … what do you think happens? And we’re doing a study on this.
Is it true you should not operate on children until their bones are finished developing? Is that sort of an old school philosophy?
No, it’s an old school philosophy. Just throw it out the window.
How can you find a foot and ankle surgeon, one who really knows what they’re doing on the CMT foot,
I want people to come here if they can. I’m amazed but I admire that COVID is not stopping anyone. Tomorrow there’s a girl from Texas and she’s driven up. There’s a boy next week from New York, and he’s flying in, you know. So it doesn’t seem to stop anybody much for the CMT and they think it’s a good time, right, because schools are virtual. So all of a sudden someone’s saying, well, this is not worth it to be freshman in college for seventy thousand dollars a year. I’m gonna get my feet taken care of. People come, I want them to stay. A lot of surgeons wouldn’t want that, but I want the person to stay here for two weeks.
Now it’s a big city and a lot of people have relatives and I would say what I tell everyone. You can get a hotel out of town for $59 somewhere a week and you can get a hotel in town for $5,900 a night, and I’ve had both types of patients. Normally the former than the latter but you stay and then the sutures will come out in two weeks and then you go home. Insurance will … we’ve never been denied insurance because most … if you’re in North Dakota … in your town the insurance knows that there’s nobody who’s going to want to do this, and if they do want to do it, the patient will say doctor how many have you done? Have uoi done hundreds of patients, the way they have at Cedars? It’s too difficult a surgery to take on you know so the the surgeons don’t want it. Even the HMOs will allow people that … one of those people I showed you is from an HMO, which is very restrictive healthcare, right, in Hawaii but the HMO doctor doesn’t want to do it. Medicaid and the medical patients aren’t allowed to come but almost all insurances will allow this.
I’m an employee. I don’t get a penny from doing the surgery, just not a penny. I’m an employee of Cedars and Cedars is part of almost all plans. And the last thing I would just say is if somebody doesn’t allow you to come at first, they will because all you have to do is say this is where I want to go. Are you willing to take the responsibility, doctor, insurance plan, but I’m not going to do well. And the answer for that 99% of the time would be, why don’t you go to Los Angeles? Now there are certainly people who do what I do in the United States, but they’re large areas where they’re not. Okay, that’s a really helpful answer. Great to know. I just said the cash price is just insurmountable. I just … it’s tens and tens of thousands of dollars. So you really need to to go through insurance and get that.
So in that regard we’ve never had anyone turned down. Sal Rosette, my surgery scheduler … I was working late night in the office, he was leaving late and I asked Sal about this. And he said to me is exactly what he said. I don’t know if it’s true or not. He said, Doc, he goes, we have no one ever turned down by insurance for you. Each doctor has something called an NPI number that designates them. He said he’s at the insurance company I’m talking to them on the phone and they say well what’s his NPI number and it’s CMT and the insurance just immediately says, oh yeah, you can go there. I don’t know if … I don’t know if he’s just reading into that or not. I said, so they’re tracking us with CMT and my doctor number? He goes. ” they must.” Blue Cross, he said … I don’t know if it’s true … but according to him he said Blue Cross knows about you and CMT. Anyway that’s a long answer. That’s okay, very helpful. Back to the age a little bit, and I know you spoke to the crooked foot being, you know, of surgical possibility at any age.
What are your thoughts on ankle fusion?
There was a consortium in Europe which you know about. Dr. Shy was there and others looking at this, the surgical issue, and we met and I was amazed that one of the surgeons there does a lot of CMT surgery said we do fusions in everyone. We do tendon transfers and fusions.
So I was born with a fusion You can do okay with the fusion of the joints that are usually involved with CMT, but you’re not perfect. And I had … if my foot moved perfectly, I would not have dislocated my ankle when I fell in the pool recently. You don’t want to do a fusion in a young person. If you have to, it’s not the end of the world. Let me tell you, if anyone’s telling you who has CMT that you need an ankle a fusion, you need another opinion from out of town.
But never fuse an ankle in a CMT patient as a general rule. Why? Because you’ll do much better with those braces. When you fuse the ankle, you take all the spring out of the ankle and you negate the ability of using those wonderful braces, those ground reaction force braces that are made now, and those braces are anything from over the counter or basically online to ten twelve thousand dollars a pair, so there’s a lot of options. But you have options unless you get your ankle fused.
Who should do my surgery?
There are orthopedic foot and ankle specialists. That’s who you want to see. An orthopedic MD foot and ankle specialist … M-D, someone who went to medical school. You know, that’s the first thing. Not a podiatrist. If there’s a podiatrist out there who’s done 100 CMT surgeries, then fine, I have no problem with that. You know, podiatrists are not medical doctors. There’s some natural competition between orthopedic surgeons and podiatrists.
I’ve operated on always over 40 000 people with CMT. Wow. In this one you need somebody with gray hair. I am so much better at this than I was 15 years ago. Go see somebody. Contact me if you want. Set up a telemedicine visit, and I’ll tell you whether I agree with your opinion or not.
And I know everybody, and I’ll secretly tell you if I think it’s a good person to go with.
The Consensus Paper – Take that paper, put it in your pocket bring it to your surgeon … learn it. CMT patients are pretty smart people. And learn what’s in that paper. Ask a few questions and see what the answers are. What we wrote in that consensus patient paper will change and it’s not the final answer, but it’s a very good start to knowing who the right surgeon is for you, right?
Elizabeth: I can’t thank you for being so passionate about our cause, and you’re very approachable, and even in the world of orthopedic surgeons. And it’s you guys are very very busy, and very task oriented, but you care. You have heart. You have soul. You follow up with your patients. I mean, the quality of care that you give is amazing. So not only are you a very competent surgeon, but also you’re somebody that’s approachable and you can talk to and you’re interesting. And so A+. Thank you so much. Thank you so much for this wonderful presentation and caring about our community.